Choosing a Non-hormonal Birth Control That’s Right For You
Choosing the right birth control for your body can be challenging. To make life just a little bit easier, I want to give you a rundown of some non-hormonal birth control options and talk about the benefits and downfalls of each. Reasons women choose to avoid hormonal birth control may be linked with concerns about negative physical side effects, changes in mental health, hormonal contraceptive-induced amenorrhea, adverse impact on sexual health, infertility, and a want to be more naturalistic.

Whatever the reason you’ve decided to investigate non-hormonal birth control options, the decision is yours & the best choice is an informed choice. So, let’s look at what options there are for non-hormonal birth controls and see which one is the best fit for you.
Withdrawal
Also known as the “pull-out method”. This method refers to pulling out the penis from the vagina prior to ejaculation.
Pros:
- No pre planning is required. Not a lot of effort needs to go into this method because you simply have your partner pull out before ejaculation to prevent any sperm getting into the vagina.
- This option is completely free. There is no need to worry about costs of acquiring birth control.
Cons:
- This method is only about 73% effective in preventing pregnancy.
- The withdrawal method can be tough to stick with. Disrupting intercourse directly before ejaculation can be challenging in the moment.
- This method requires you to put the responsibility in someone else’s hands. You must rely on your partner to have control over his timing of pulling out. Even with the most conscientious partner, it can be difficult to time the withdrawal correctly.
This method could be a good option for someone who prioritizes flexibility, is ok with the possibility of pregnancy, and wants to avoid putting any foreign objects or chemicals in their body. This method provides convenience but not reliability and may be a good fit for someone that’s not ready to commit to something a little more comprehensive.
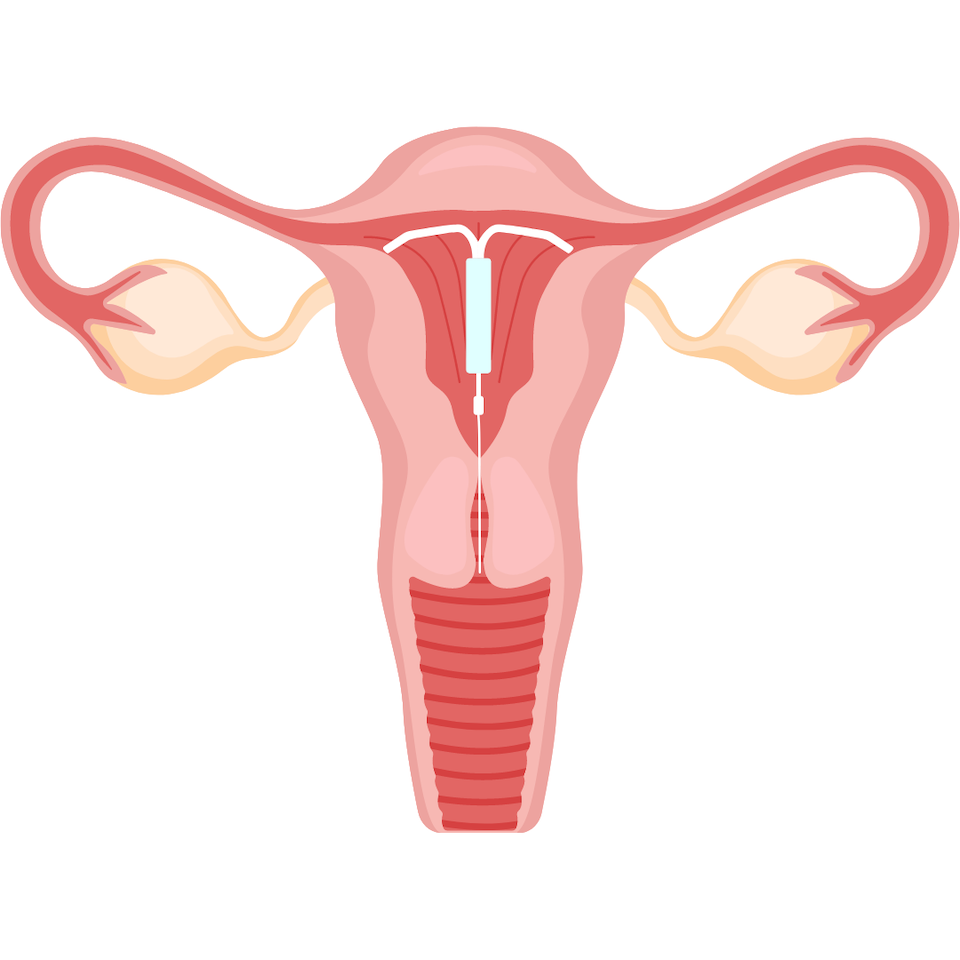
Copper IUD
The ParaGard copper IUD is a long term non-hormonal birth control option. The IUD is a small device made of flexible plastic and metal that is placed in the uterus. Insertion of this device requires an in-office procedure. This device acts as a blocking mechanism to block the sperm from entering the uterus.
Pros:
- The IUD is highly effective
- This method has a 99% effective rate. Your chances of getting pregnant with this method are low.
- The IUD offers convenience and low maintenance. Once the IUD is placed there is no need to take it out for up to 10 years unless you are ready to try a new method, get pregnant, or are having health concerns.
- Cost-effective. Typically, this device is covered by insurance and since you only need it placed once, there’s no further costs after the initial insertion of the device.
Cons:
- Painful insertion. Many women experience cramping when the device is inserted, and this may last for the first few days to weeks.
- Increased menstrual symptoms. After the device is inserted, many women experience heavier menstrual flows and increased menstrual cramps.
- Risks of potential perforation or embedding of the IUD in the uterus. This is rare but could be potentially serious.
- Risk of copper toxicity.
This option could be good for someone who highly wants to avoid pregnancy for a longer time frame, is ok with managing heavy flow periods and more intense pain with cramping, lives a busy life, and doesn’t want to worry about closely managing their birth control.
Diaphragm
Diaphragms are dome-shaped latex or silicone barriers that you insert into your vagina and sit over your cervix. It’s recommended to see a clinician to get the right fitting and instructions before use. This method can be used conjunctively with spermicide, a chemical gel, foam, or jelly that kills sperm.
Pros:
- The diaphragm method is around 84% effective and when paired with spermicide, this method can be up to 94% effective.
- The diaphragm is relatively inexpensive and reusable.
Cons:
- This method can be burdensome. A diaphragm needs to be placed properly in the vagina before intercourse and must be left in place for at least six hours after. If you are using spermicide with the diaphragm, then it adds an additional step before intercourse.
- Requires a lot of maintenance. After using the diaphragm, you need to be sure to clean it, dry it, and store it properly.
- Doesn’t leave much room for spontaneity. Carrying around spermicide and a diaphragm might feel a little awkward. You must pause, add spermicide, and insert your diaphragm at least an hour before intercourse.
- Diaphragms may increase risks for UTIs and should be avoided by someone who may be prone to UTIs.
This option may be a good fit for someone that lives a more regimented life, is ok with managing a higher maintenance method, and wants to maintain more control of their birth control method.
Condoms
Condoms are one of the more popular non-hormonal birth control methods. Condoms are mainly made from latex, but some are made from polyurethane.

Pros:
- Condoms are the only form of birth control that protects against STDs. Reducing the worry about contracting an STD can provide great relief and reduce stress involving sexual activity.
- Condoms provide convenience. There is minimal preplanning, they are easily obtainable and easy to use.
- Condoms are fairly effective. Effectiveness against pregnancy can vary from 80% to 98% depending on proper use.
Cons:
- Condoms may decrease sexual sensitivity. Women and men may feel less inclined to use condoms because they feel they decrease sexual satisfaction.
- Condoms may cause irritation or allergies due to the latex material.
- The effectiveness of using condoms relies on the proper use of the condom and even with proper use, there is always the possibility of breakage.
This option could be a good option for someone who prioritizes convenience, has multiple partners, wants to reduce STD risks, and wants to spend less time managing their birth control.
Fertility awareness
The main concept for fertility awareness is tracking your menstrual cycle to determine when you are ovulating. The varying methods in fertility awareness focus on calendar tracking, basal body temperature tracking, and cervical mucus methods to determine ovulation time.
Pros:
- Can help you become more mindful and in sync with your body’s natural rhythms.
- Doesn’t require you to put anything foreign in your body. No gels, no latex, no painful insertion of devices.
- There are many apps, services, and testing strips available to help you manage and track your cycle.
- Greater involvement of your partner to avoid pregnancy.
- Can be up to 95% effective when managed correctly.
Cons:
- If not managed accurately, it can have a low effective rate.
- Requires good management skills. For this method you need to be on top of tracking and documenting your cycle, checking basal body temperatures and cervical secretions.
- May require you to be abstinent for a large window during your cycle when you are fertile, as many as 10–14 days per month.
- Not very effective for women who have irregular or unpredictable menstrual periods.
- Thyroid conditions, illness and alcohol intake can all impact basal body temperature results which may make it challenging to accurately track.
This method is good for someone who prioritizes avoiding altering their body’s natural rhythms, has good management skills, wants to avoid adding anything foreign to their body, and wants to increase fertility involvement of their partner.

Services to help you track:
- Clue period tracker: ovulation calculator, fertility predictions, and cervical fluid tracker.
- Natural Cycles birth control: determines fertility status based on basal body temperature analysis.
- Daysy tracking thermometer: A device that takes your basal body temperature and menstruation data and calculates for you when you are fertile and when you are not.
Phexxi
Phexxi is one of the newest FDA-approved non-hormonal birth controls released on the market. Phexxi is a prescription vaginal gel that lowers the pH in your vagina which inhibits the sperm from movement. You insert the dose of Phexxi into your vagina before intercourse.
Pros:
- This method is 86 -93% effective and can be paired with condoms or diaphragm to increase effectiveness.
- Ease of use. This method comes in an applicator similar to a tampon and just needs to be inserted within one hour of intercourse
- Convenience. You can use this method when you need it, it’s easy to carry on you, and there is little pre-planning that goes into using this method
Cons:
- This method is expensive if your insurance doesn’t cover it, $250 – 275 for 12 doses.
- A small percent of women have experienced burning, itching, or discomfort.
- You must insert a dose before every instance of intercourse so if you want to have multiple interactions you must first insert another dose.
This method is a good fit for someone who prioritizes convenience, doesn’t have cost barriers, and isn’t ready to commit to a more long-term method or a method that needs more self-management.
So which method is right for you? The birth control option that fits you best depends on which method you can be most consistent with. If you are currently on hormonal birth control and are thinking about transitioning to a non-hormonal option, it’s important to prepare your body for this transition. By having a plan in place for coming off hormonal birth control, you will decrease unwanted symptoms like acne, weight gain, or PMS. To learn more about what steps to take when you are planning to come off birth control, check out our mini course Balance Your Hormones Naturally After Birth Control here.
Written by: Nicole Morgan
Instagram: noticeably_nourished
References
Cornell Health. (2021, July). Intrauterine device (IUD) – Cornell health. The Intrauterine Device. Retrieved January 12, 2022, from https://health.cornell.edu/sites/health/files/pdf-library/Intrauterine-Device.pdf
Cornell University. (2019, October 18). Non-hormonal methods contraception – Cornell Health. Cornell health. Retrieved January 12, 2022, from https://health.cornell.edu/sites/health/files/pdf-library/non-hormonal-methods-contraception.pdf
Fulton, A. (2021, October 28). Hormonal vs. non-hormonal contraception: What’s the difference? HealthyWomen. Retrieved January 12, 2022, from https://www.healthywomen.org/created-with-support/hormonal-vs-non-hormonal-contraception/particle-5
Le Guen, M., Schantz, C., Régnier-Loilier, A., & de La Rochebrochard, E. (2021). Reasons for rejecting hormonal contraception in western countries: A systematic review. Social Science & Medicine, 284, 114247. https://doi.org/10.1016/j.socscimed.2021.114247
Parenthood, P. (2018, February 1). What are the best birth control options that aren’t hormonal? Planned Parenthood. Retrieved January 12, 2022, from https://www.plannedparenthood.org/learn/teens/ask-experts/what-are-the-best-birth-control-options-that-arent-hormonal
Staff, N. W. H. N. (2020, August 5). Fact sheet: PHEXXI contraceptive gel: National Women’s Health Network. National Women’s Health Network |. Retrieved January 12, 2022, from https://nwhn.org/phexxi/
UC Davis. (2019, June 17). Fertility awareness. Fertility Awareness | Student Health and Counseling Services. Retrieved January 12, 2022, from https://shcs.ucdavis.edu/health-topic/fertility-awareness
Comments +